|
HPI:
The patient is a 41-year-old female with past medical history of diabetes who presents with right knee pain. Patient states that approximately 2 days ago, she noticed that her knee was red, swollen, and has gotten sore to the point that she cannot walk. Patient denies ever having symptoms like this before. Patient denies any prior surgeries or trauma to the joint. Physical exam: Swelling and erythema over the right knee. The patient is unwilling to walk in the exam room stating that she cannot secondary to pain. The knee is warm to the touch with no overlying induration. The patient has limited active and passive range of motion secondary to pain. Patient has 2+ distal pulses with intact sensation to light touch in all dermatomes. Radiographs: Normal knee Laboratory data: CBC: WBC 24K, Platelets 224 Serum glucose: 197 ESR: 39 CRP: 7.2 Joint aspiration: cloudy fluid, WBC 62K, gram stain negative, glucose 94 Diagnosis and Plan: Septic arthritis. Patient was started on vancomycin and orthopedics was consulted. She was admitted to the hospital and taken to the OR later that night for washout. Discussion: Location: The most commonly affected joints in descending order are the knee (>50%), hip, shoulder, elbow, ankle, sternoclavicular joint. Risk Factors: Greater than 80 years of age, presence of prosthetic joint, overlying skin infection, diabetes, rheumatoid arthritis, cirrhosis, HIV, history of gout or pseudogout, endocarditis, recent bacteremia, IV drug user, recent joint surgery. Organisms: Most common in all patients is Staphylococcus aureus which accounts for greater that 50% of infections. There are some specific patients that have high rates of other organisms that we should be aware:
ER Work-up:
Differential: An emergency physician is only as good as the differential that they consider, therefore, we should maintain the following on their differential: gout, pseudogout, reactive arthritis, rheumatoid arthritis, Lyme disease, gonococcal arthritis, traumatic arthritis, cellulitis, bursitis. Treatment: There are no good randomized controlled trials for antibiotic treatment of septic arthritis. Current recommendations are based on the most likely organism. If you lucky enough to have a positive Gram stain, then you should treat gram-positive smear with vancomycin and gram negative smear with a third generation cephalosporin such as ceftriaxone. Other specialized considerations are:
Finally, once confirmed, orthopedic service should be consulted as these joints will need washout in the operating room. Pearls:
0 Comments
HPI: Otherwise healthy 27-year-old male who presents with right knee pain. The patient is a construction worker and while on a construction site today, a wooden wall fell onto him and other workers. The patient received an isolated injury to his right knee and presents with pain and deformity. Patient denies any other injuries, his vital signs are within normal limits. Exam: Patient lying in a supine position. Right knee has no significant effusion, erythema, or overlying abrasions/lacerations. Palpation of the right knee reveals a large step off between the patella and anterior surface of the femur. Patient is neurovascularly intact distally. Representative x-ray is shown below. http://radsource.us/ Discussion: There are 5 different types of knee dislocations based on the direction of displacement from the tibia.
Physical exam often times result with no obvious deformity. It has been estimated that as many as 50% spontaneously reduce prior to arrival to the ED. In the emergency department, vascular examination is of utmost importance. With obvious deformity and absent pulses, reduction must take place immediately, before radiographs are obtained. After reduction, dorsalis pedis and posterior tibial pulses should be palpated, but the palpation of pulses does not rule out arterial injury. The next step should be measuring ankle-brachial index of the affected side. If the ABI is normal (> 0.9), then you can monitor the patient with repeat examinations as this has a 100% negative predictive value for arterial injury. If the ABI is abnormal (<0.9), then a CT angiography should be performed along with vascular surgery consultation. If pulses are still not palpable after successful reduction, immediate surgical exploration should be performed. There is one situation where reduction of the knee should not take place. The “dimple sign” represents buttonholing of the medial femoral condyle through the anterior medial joint capsule. The sign indicates an irreducible dislocation and closed reduction is contraindicated for the risk of skin necrosis. http://jbjs.org/content/87/7/1571
Initial imaging consists of plain radiographs. Remember, many of these reduce prior to arrival and the radiograph may appear normal. Despite this, you should look closely for avulsion fractures and osteochondral defects. CT angiography should be obtained as discussed above if necessary. After reduction and verification of ABI, the patient should be placed in a splint with 20-30° of flexion. Post reduction films should be taken after the splint or brace is applied to confirm placement. If emergent surgical intervention is not warranted, many of these require delayed ligamentous repair. Long-term complications consist of arthritic symptoms, instability of the joint, peroneal nerve injury, and chronic vascular compromise. Management Pearls:
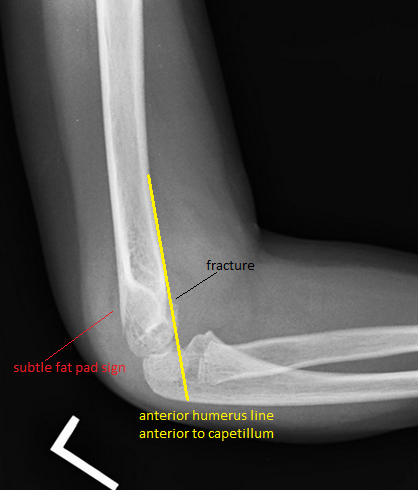
References: 1. Patel, Anay. "Knee Dislocation." Orthobullets 08/11/15. Retrieved 10/15/15 from http://www.orthobullets.com/trauma/1043/knee-dislocation. 2. Peskun, C.J. et al. "Diagnosis and Management of Knee Dislocations." The Physician and Sportsmedicine. Dec, 2010. 4:38, pages 101-111. By Dr. Phillip Lunsford HPI: Approximately 5 y/o male presents with right elbow pain and refusal to move the right arm after falling from a chair on an outstretched arm. EXAM: Gross deformity present on the distal humerus, just proximal to the elbow with mild skin tenting and tenderness. Refusal to move the elbow joint. Unable to extend the wrist and digits. Remainder of exam normal. IMAGES: Obtain AP and lateral elbow views Normal Elbow: anterior humerus line intersects the middle third of the capitellum Gartland Classifications: Garland Type 1: Non-displaced Garland Type II: Displaced with posterior cortex intact Garland Type III: Completely displaced
MANAGEMENT: #Non-operative - Posterior long arm splint with less than 90 degrees of flexion - Type I and some Type II fractures. - Consult Ortho for Type II fractures to determine if operative management is needed #Operative - All Type III fractures, some Type II fractures - “floating elbow” : ipsilateral supracondylar and forearm fractures - Immediate operative management if vascular compromise is present - Reduce in ER if any vascular compromise is present - Most are admissions with next day operative fixation DISCUSSION: - Incredibly common in 5-7 year olds with a fall on an outstretched arm. - Radial, ulnar, anterior interosseous nerve neurapraxia all very common and resolve with reduction without long term effects but require expedited management - Very easy to miss a type I fracture, use the anterior humerus line and fat pad sign - Garland classification above, determines management - Can be associated with vascular injury (~1%), this requires immediate reduction KEY POINTS: - Use the anterior humerus line and fat pad sign to help find subtle fractures - High suspicion in any fall on an outstretched arm - Remember the Garland Classifications - Most Type II and all Type III will require operative management and admission - A posterior long arm splint for Type I fractures - Always assess for neurovascular compromise By Dr. Mohamed El-Kara HPI: Middle age man s/p MCC with open fracture of right leg. Tourniquet applied in the field. Physical Exam: Completely shattered tibia and fibula with 10cm open wound. Weak but palpable DP after taking tourniquet down. Intact sensation to light touch in superficial peroneal, deep peroneal, and tibial distributions. Able to wiggle toes and slight dorsiflexion. Management: Basic Management of Open Fractures
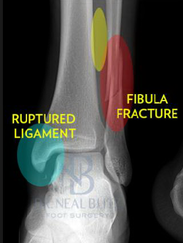
HPI: Middle age male who presents with left ankle pain, swelling, and deformity s/p fall down stairs. Unable to bear weight to LLE. Physical Exam: obvious deformity, edema, ecchymosis to L ankle. TTP over medial and lateral malleolus. Unable to flex and extend at ankle 2/2 pain. DP/PT 2+. Normal sensation to light touch to dorsal surface/plantar surface/1st web space. IMAGING: Diagnosis and Management: This patient has a Weber B distal fibula fracture with medial subluxation of the tibia and disruption of the mortise joint. Combination of distal fibula fracture and likely complete disruption of deltoid ligament is a bimalleolar fracture-dislocation equivalent. Thus, this is an UNSTABLE ANKLE! Patient’s ankle was reduced using axial traction and inversion, placed in posterior sugar tong splint. Injury required 3 reductions, which is common due to the instability of this injury. Patient was admitted to Orthopedic Trauma service and scheduled for next day ORIF.
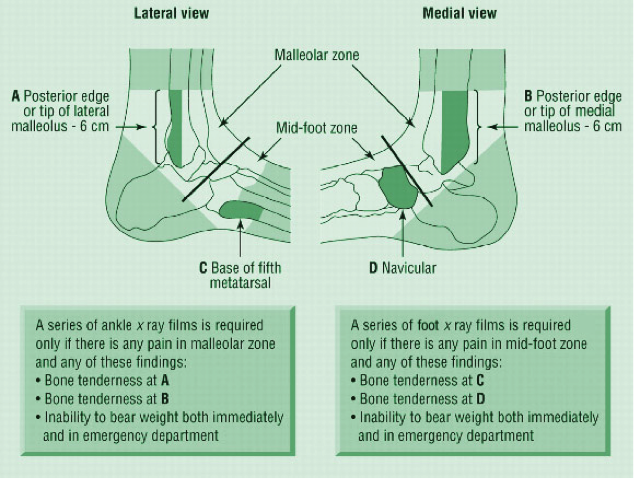
HPI: Middle-aged male s/p MCC. PE: Ecchymoses, swelling, and tenderness about ankle. Tender over proximal fibula and pain with squeezing of calf. Figure 1: Mortise view of ankle showing widened mortise mediallyFigure 2: Leg film showing proximal fibular fractureAnkle Sprains: - Divided into grades o I: Minor, no significant ligamentous damage. Able to bear weight. o II: Associated with partial ligamentous tear. Significant ecchymoses/swelling. Difficulty bearing weight. o III: Associated with complete ligamentous tear. Significant functional loss and universal inability to bear weight. - When should we obtain radiographs?: o If pretest clinical suspicion is high based on mechanism of injury or patient cannot be ruled out for fracture based on Ottawa ankle rules: Syndesmotic injuries (AKA “high” ankle sprains):
o PE and mechanism:
o Treatment:
- Otherwise patient needs syndesmotic screw fixation. Patient can be immobilized and follow-up as an outpatient for surgical fixation HPI: Patient 1: Restrained passenger of a head on MVC. Patient 2: Elderly patient with fall from standing. Physical Exam: Patient 1: Hip flexed and internally rotated. Unable to straighten the leg. Unable to walk. Patient 2: Hip flexed and externally rotated. Unable to straighten the leg. Unable to walk. Imaging: Patient 1: Posterior hip dislocation of native hip. Patient 2: Superolateral hip dislocation of prosthetic hip. Posterior Hip DislocationProsthetic Hip DislocationTreatment:
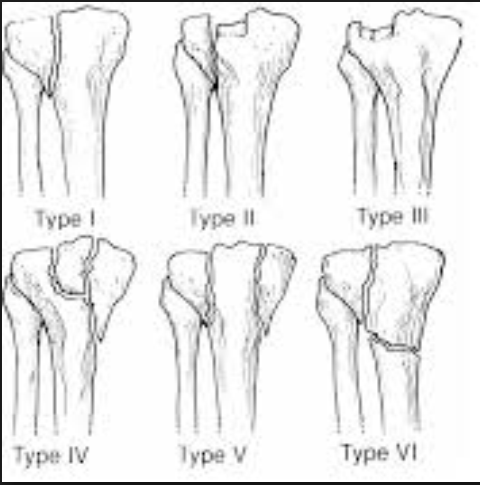
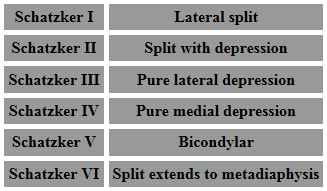
****Don't forgot you can find the ED Policy for Deep Sedation on the Top 20 Page. Anesthesia must be present for intubation. Click here to read more. HPI: Patient 1: Restrained MVC. Presented with knee pain and swelling. Patient 2: Fall from height and chief complaint of shoulder and knee pain. Physical Exam: Patient 1: Swollen left knee with tenderness to palpation. Patient 2: Knee visibly deformed, swollen, and bruised. Small open deformity w/ active bleeding. High risk for compartment syndrome. Imaging: Patient 1: Schatzker type 2 fracture (see table below for classifications of Schatzker fracture) Patient 2: Schatzker type 6 fracture Dispo: Patient 1: Admitted. Splinted w/ ORIF as inpatient. Patient 2: Admitted. Splinted w/ closed reduction and external fixation. Plan for definitive repair in ~2 weeks after soft tissue swelling has subsided. Treatment: 1) Hinged knee brace w/ passive ROM - for patients w/ minimally displaced or split depressed fractures or minimal baseline mobility. 2) External fixation - for patient w/ open or comminuted fractures or significant soft tissue swelling. 3) ORIF - for >3mm articular step off or varus/valgus instability. Types of Schatzker Fractures:
HPI: Patient presents with a grossly deformed right upper extremity.
PE: Gross deformity of humerus, no open fracture. Unable to extend wrist. Unable to hyper-extend MP joints of fingers and unable to flex IP joint of thumb. Radial and ulnar pulses intact. IMAGING: Multi-factorial fracture along the mid third of humerus along the expected course of the radial nerve. DISPO (if at free standing ED): Transfer patient to ED with on-call orthopedics for definitive fixation. Reduce and splint prior to transfer. TREATMENT: Nonoperative managment. Splinted and cast at bedside. Follow radial nerve palsy clinically for improvement. |
Orthopedics BlogAuthorCMC ER Residents Archives
June 2018
Categories
All
Disclaimer: All images and x-rays included on this blog are the sole property of CMC EM Residency and cannot be used or reproduced without written permission. Patient identifiers have been redacted/changed or patient consent has been obtained. Information contained in this blog is the opinion of the author and application of material contained in this blog is at the discretion of the practitioner to verify for accuracy.
|
















 RSS Feed
RSS Feed
