|
HPI: 18 yo male involved in a head on MVC. Patient was the unrestrained driver. The patient was initially unconscious but is now combative. Per EMS there is an obvious deformity to the right lower leg with “bone sticking out.” Patient is slightly tachycardic on arrival with a HR of 102 with a blood pressure of 132/90 and has a GCS of 15. EXAM: The primary survey is unremarkable and the patient continues to maintain stable vital signs. During the secondary survey a 3 cm laceration with what appears to be protruding bone is noted 20 cm distal to the R knee. Patient has intact sensation distal to the injury with strong DP and PT pulses with good capillary refill. Steady dark bleeding is noted from the wound. The motor exam is limited by pain and uncooperative patient. IMAGING: MANAGEMENT: 1. First priority is trauma resuscitation 2. Thorough neurovascular examination 3. Irrigation and debridement of the site 4. Application of a splint to the affected limb for temporary stabilization 5. In addition to standard trauma resuscitation tetanus prophylaxis and early administration of antibiotics is indicated
DISCUSSION: - Patients will need operative debridement and fixation of their fractures - Copious irrigation in the OR is key for preventing infection - Direct pressure, NOT blind clamping is the best way to control bleeding - Open fractures can often wait until the following day for operative repair. At one time it was thought every open fracture required operative repair within 6 hours to lower the risk of infection. This is NOT true. KEY POINTS: - Tetanus and early antibiotic administration a MUST.
- Thorough neurovascular examination prior to splinting - Remove gross debris from fracture site and cover with moist gauze. - Does not require immediate operative repair - Apply temporary splint to stabilize fracture
0 Comments
HPI: 27 yo male playing basketball “jammed” his right ring finger which was immediately followed by pain, shortening of the digit and inability to flex his finger. Exam: Obvious deformity at the right ring finger PIP joint with associated ecchymosis. Sensation to light touch intact and good capillary refill at the affected finger. Patient unable to flex at affected digit. No other identifiable injuries noted. Images:
Discussion:
Management:
Key Points:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696003/
Orthobullets.com HPI: 35 yo male construction worker falls from 15 feet off of a ladder complaining of severe R foot/ankle pain as well as lower back pain. Exam: Obvious swelling and ecchymosis of the R ankle and heel with associated tenderness. No deformity or tenderness to the L foot/ankle. Midline lumbar tenderness. Patient has palpable PT/DP pulses bilaterally with no noted sensory deficits. Images: Tongue type: (Credits: South Florida Institute of Sports Medicine) Bohler’s angle (normal): Bohler’s angle (reduced): (Radiopedia.org) Management:
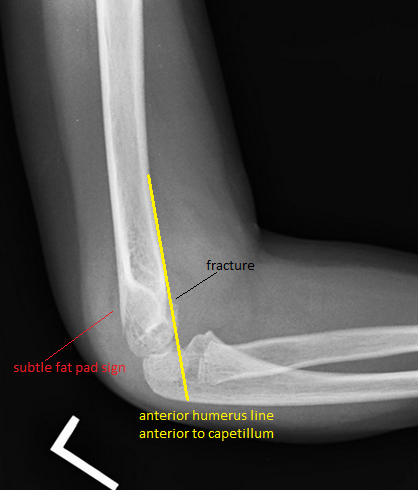
#Initial ED - Obtain AP, Lateral, oblique foot plain film images at minimum. - Often Broden, Harris views will be requested for complete visualization. #Non-operative - Extra-articular fractures with minimal displacement and intact Achilles tendon. - Sanders Type I fractures - Bulky cast with extra padding around the heel and ankle. - Requires EXTENDED non-weightbearing status. Often approaches 12 weeks. - All require referral to orthopedic surgery #Operative - Prompt recognition of Tongue-type fractures as illustrated above. - Orthopedic EMERGENCY as skin overlying the fracture has a high instance of compromised vascularity and death/necrosis. - Displaced intraarticular fractures - Sanders type II-IV Discussion: - Common in males aged 35-45, often work related - Due to extended non-weightbearing requirement these injuries have large socioeconomic impact on patients - High complication rate if not recognised early - Contralateral calcaneus and spine have a 10% concomitant injury rate. - Look for reduced Bohler angle and increased angle of Gissane Key Points: - Be vigilant as secondary injuries very common - Most commonly the spine and contralateral calcaneus - Recognise tongue-type fractures early and prompt notification of orthopedic surgery - Don’t forget the spine in axial load type injuries References: http://www.orthobullets.com/trauma/1051/calcaneus-fractures HPI: Approximately 5 y/o male presents with right elbow pain and refusal to move the right arm after falling from a chair on an outstretched arm. EXAM: Gross deformity present on the distal humerus, just proximal to the elbow with mild skin tenting and tenderness. Refusal to move the elbow joint. Unable to extend the wrist and digits. Remainder of exam normal. IMAGES: Obtain AP and lateral elbow views Normal Elbow: anterior humerus line intersects the middle third of the capitellum Gartland Classifications: Garland Type 1: Non-displaced Garland Type II: Displaced with posterior cortex intact Garland Type III: Completely displaced
MANAGEMENT: #Non-operative - Posterior long arm splint with less than 90 degrees of flexion - Type I and some Type II fractures. - Consult Ortho for Type II fractures to determine if operative management is needed #Operative - All Type III fractures, some Type II fractures - “floating elbow” : ipsilateral supracondylar and forearm fractures - Immediate operative management if vascular compromise is present - Reduce in ER if any vascular compromise is present - Most are admissions with next day operative fixation DISCUSSION: - Incredibly common in 5-7 year olds with a fall on an outstretched arm. - Radial, ulnar, anterior interosseous nerve neurapraxia all very common and resolve with reduction without long term effects but require expedited management - Very easy to miss a type I fracture, use the anterior humerus line and fat pad sign - Garland classification above, determines management - Can be associated with vascular injury (~1%), this requires immediate reduction KEY POINTS: - Use the anterior humerus line and fat pad sign to help find subtle fractures - High suspicion in any fall on an outstretched arm - Remember the Garland Classifications - Most Type II and all Type III will require operative management and admission - A posterior long arm splint for Type I fractures - Always assess for neurovascular compromise By Dr. Mohamed El-Kara |
Orthopedics BlogAuthorCMC ER Residents Archives
June 2018
Categories
All
Disclaimer: All images and x-rays included on this blog are the sole property of CMC EM Residency and cannot be used or reproduced without written permission. Patient identifiers have been redacted/changed or patient consent has been obtained. Information contained in this blog is the opinion of the author and application of material contained in this blog is at the discretion of the practitioner to verify for accuracy.
|









 RSS Feed
RSS Feed
