|
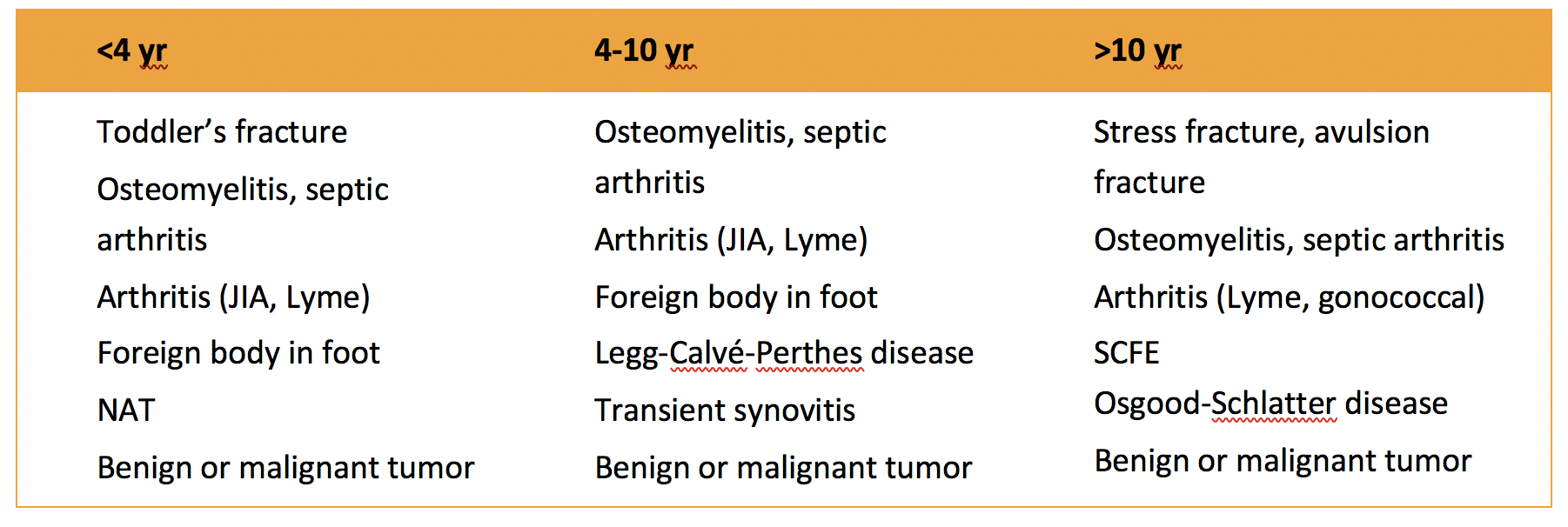
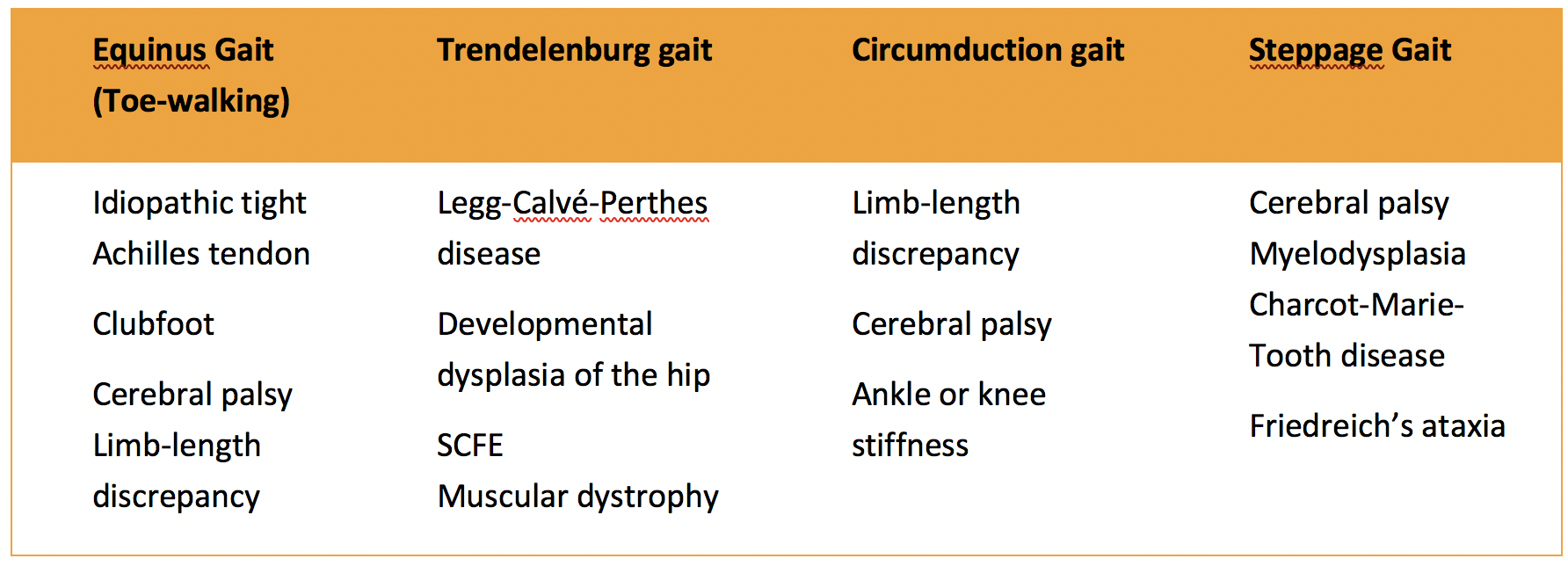
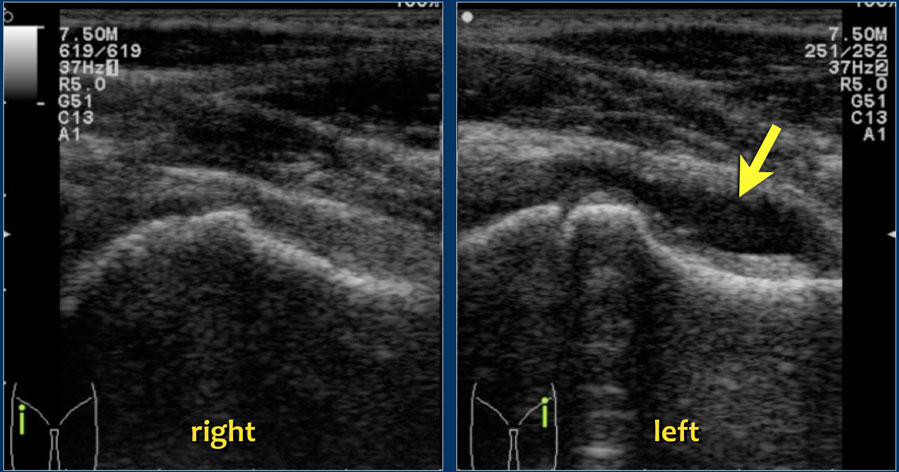
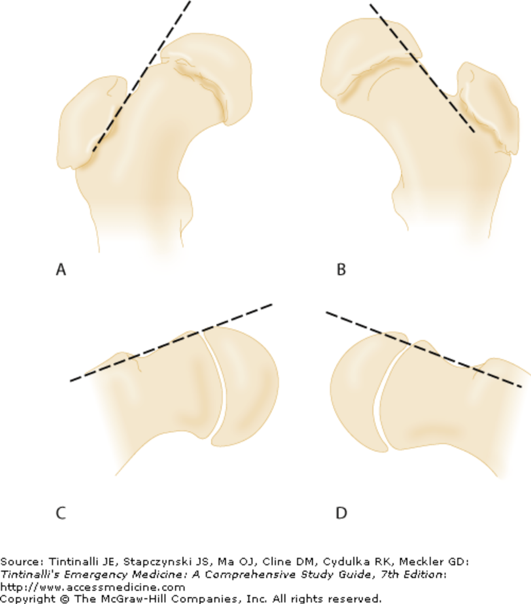
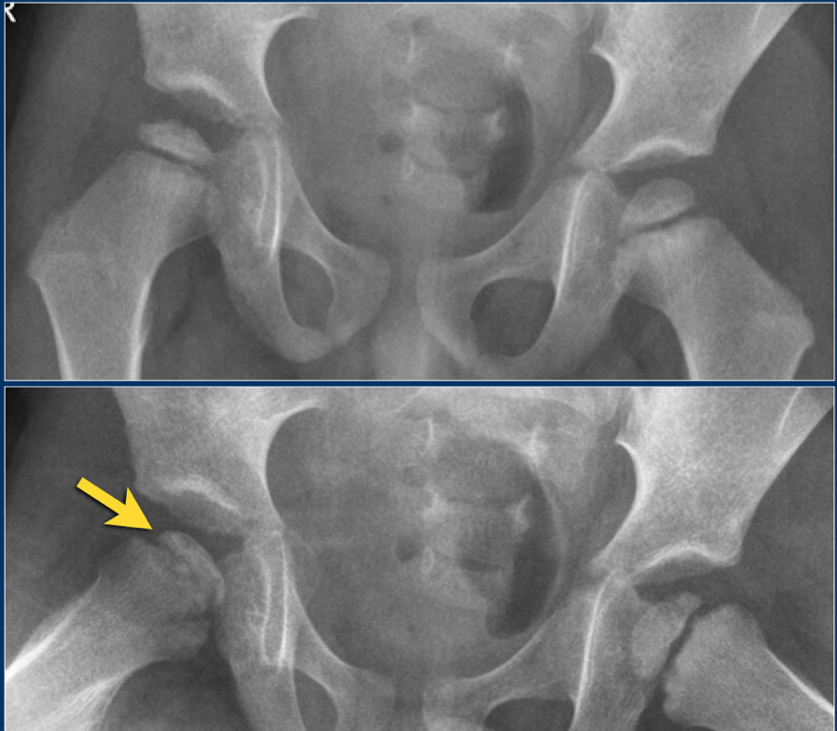
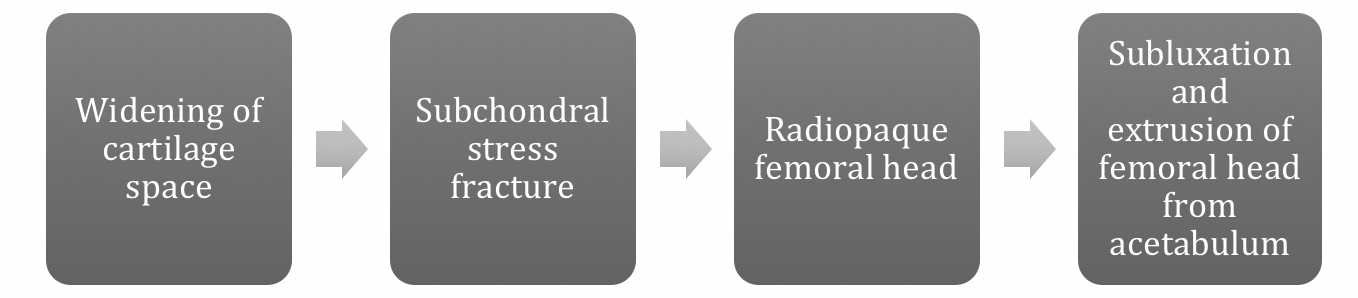
Authored by Dr. Jessica Hoglund 1. Differential (categorized based on gait pattern) A. Antalgic gait B. Non-antalgic gait 1. Transient synovitis A. Most common cause of hip pain/limp in children <10 yrs B. Aseptic inflammation of the hip (postviral etiology) C. Diagnosis i. Physical exam: 1. Non-toxic 2. Antalgic gait i. Imaging performed when considering other differentials ii. Ultrasound may be performed to confirm the presence of a joint effusion D. Management i. Rest ii. Analgesics 2. Septic arthritis A. Causes i. Bacterial infection of joint ii. Most commonly s. aureus iii. Consider E. coli or GBS in children < 2 months iv. Consider gonococcal arthritis in adolescents, sexually active patients, and in polyarticular arthritis v. Consider salmonella in sickle cell disease B. Clinical features i. Neonates often do not appear ill and may not have fever in 50% of cases ii. Older infants, toddlers, children may localize, limp, or refuse to walk C. Diagnosis i. Physical exam1. Limb externally rotated, flexed, and abducted ii. Labs1. CBC, ESR, possibly blood cultures iii. Kocher criteria (septic arthritis vs transient synovitis, >3 predictors high risk for septic arthritis) 1. Non weight-bearing 2. Temp > 101.3oF (38.5oC) 3. ESR > 40 mm/hr 4. WBC > 12,000 cells/mm3 iv. Imaging v. Arthrocentesis 1. Ultrasound guided or fluoro guided for hip 2. Synovial fluid with >50,000 WBC’s, >75% PMN’s, positive gram stain and culture D. Management i. IV antibiotics (vanc, rocephin or cefoxatime if < 2 months) ii. Surgical drainage E. Complications i. Avascular necrosis ii. Capsule damage iii. Chronic arthritis iv. Osteomyelitis v. Sepsis 4. SCFE A. MCC of hip disability in adolescents B. Obese adolescents whose hips are exposed to repetitive minimal trauma C. Diagnosis i. Physical exam 1. Decreased internal rotation 2. Antalgic or Trendelenburg gait 3. Determine if pt is able to ambulate with or without crutches (determines prognosis) ii. Imaging 1. Any adolescent with chronic groin, hip, thigh, or knee pain deserves bilateral hip XR (AP and lateral) 2. High incidence of bilateral disease 3. Use Klein’s lines to aid in diagnosis. A and C below are abnormal. B and D are normal (line drawn from superior aspect of femoral neck transects lateral aspect of femoral head). D. Management i. Non weight bearing (important to prevent further slippage) ii. Operative management with possible prophylactic pinning of contralateral hip E. Complications i. Avascular necrosis ii. Premature closure of physis iii. Limited ROM iv. Osteoarthritis 5. Legg-calve-perthes disease A. Idiopathic avascular necrosis of proximal femoral epiphysis B. Usually unilateral (10-15% bilateral) C. Clinical features i. Insidious onset of mild hip or knee pain, possible limp ii. Repeated episodes of ischemia of femoral head à infarction and necrosis à subchondral stress fracture D. Diagnosis i. Physical exam 1. Decreased abduction and internal rotation 2. Possible thigh atrophy on affected side 3. Limb shortening (advanced cases) ii. Imaging 1. Early radiographs may be normal, but MRI will show edema in femoral epiphysis with T1 weighted 2. Radiographic progression of disease E. Management i. Symptomatic tx ii. Non weight bearing iii. Operative management may prevent early osteoarthritis can be managed non-operatively with spontaneous revascularization of femoral head F. Complications i. Osteoarthritis ii. Coxa magna deformity (short, broad femoral head and column) Flynn, John M, and Roger F Widmann. “The Limping Child: Evaluation and Diagnosis.” Journal of the American Academy of Orthopaedic Surgeons, vol. 9, no. 2, Apr. 2001.Horowitz, Diane Lewis, et al. “Approach to Septic Arthritis.” American Family Physician, 15 Sept. 2011, www.aafp.org/afp/2011/0915/p653.html.“Imaging in Slipped Capital Femoral Epiphysis .” Imaging in Slipped Capital Femoral Epiphysis: Practice Essentials, Radiography, Computed Tomography, 6 May 2017, emedicine.medscape.com/article/413810-overview.“Legg-Calve-Perthes.” Legg-Calve-Perthes - Orthopedics - Medbullets Step 2/3, step2.medbullets.com/orthopedics/120519/legg-calve-perthes.Radiology In Ped Emerg Med, Vol 4, Case 17, www.hawaii.edu/medicine/pediatrics/pemxray/v4c17.htmlSwaminathan, Anand. “Pediatric Septic Hip.” Core EM, coreem.net/core/pediatric-septic-hip/.Tintinalli JE, Stapczynski J, Ma O, Cline DM, Cydulka RK, Meckler GD, T. Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 7e; 2011 Available at:http://accessmedicine.mhmedical.com/content.aspx?bookid=348§ionid=40381606 Accessed: February 12, 2018
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Orthopedics BlogAuthorCMC ER Residents Archives
June 2018
Categories
All
Disclaimer: All images and x-rays included on this blog are the sole property of CMC EM Residency and cannot be used or reproduced without written permission. Patient identifiers have been redacted/changed or patient consent has been obtained. Information contained in this blog is the opinion of the author and application of material contained in this blog is at the discretion of the practitioner to verify for accuracy.
|



 RSS Feed
RSS Feed
