|
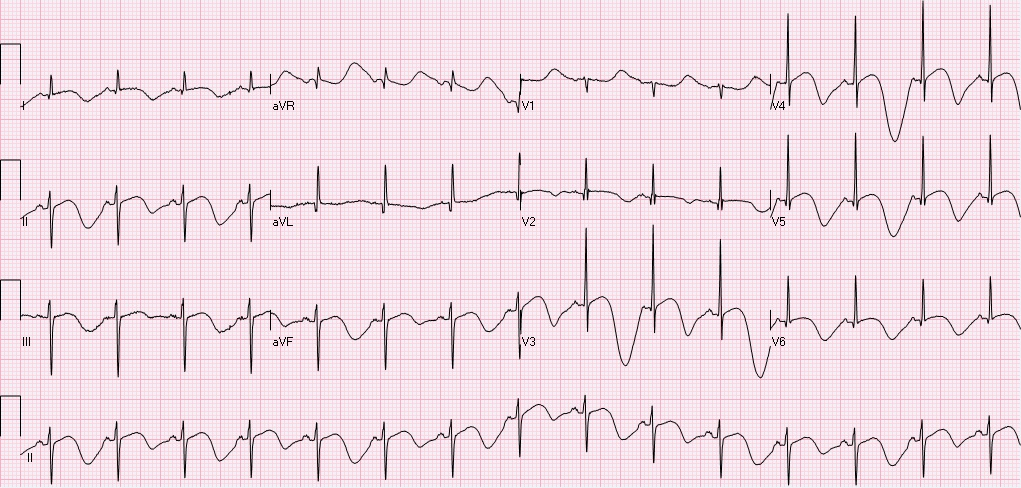
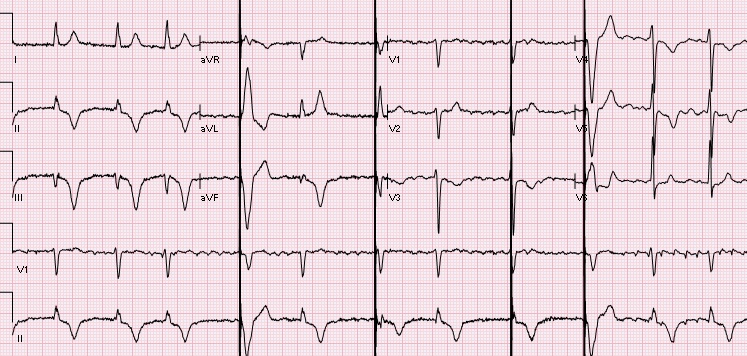
A 56 year old female with a history of asthma, hypothyroidism, tobacco use, chronic opioid use was found down at home, found to have subarachnoid hemorrhage, left temporal hematoma with bilateral supraclinoid aneurysms on CTA, s/p embolization. Hospitalization has been complicated by vasospasm, fevers, long QT, and stress induced cardiomyopathy. On hospital day 11 the following EKG was obtained to assess the patient's long QT noted on previous EKGs (500, 516, 620). Rate 89, sinus rhythm with sinus p waves, left axis deviation, normal PR, QRS intervals, prolonged QTc 732. T-wave inversions in I, II, III, aVF, V2-V6. In fact, if you pay attention to the T-wave morphology you will notice polymorphic deep t-waves, alternating in depth and morphology. There are two interesting points from this EKG: 1) T-QT pattern, and 2) T wave alternans. T-QT pattern:
T wave alternans:
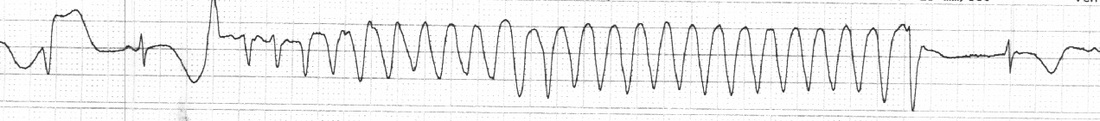
Approximately 2 hours after the above EKG, the following rhythm strip was noted on telemetry. Here you see a PVC followed by a compensatory pause, followed by polymorphic VT. Pauses are frequent triggers of Torsades. The patient went on to experience several sustained, and non-sustained runs of polymorphic VT overnight. She received aggressive Mg & K repletion, defibrillator pads were placed, but patient remained hemodynamically stable and did not require defibrillation or overdrive pacing. QT decreased and VT resolved.
Teaching points:
References: Warraich H, Buxton A, Kociol R. Macroscopic T-wave alternans in a patient with takotsubo cardiomyopathy and QT prolongations. Heart Rhythm. 2014 Oct;11(10):1848-9. Sommargren C, Drew B. Preventing torsades de pointes by careful cardiac monitoring in hospital settings. AACN Adv Crit Care. 2007 Jul-Sep;18(3):285-93
0 Comments
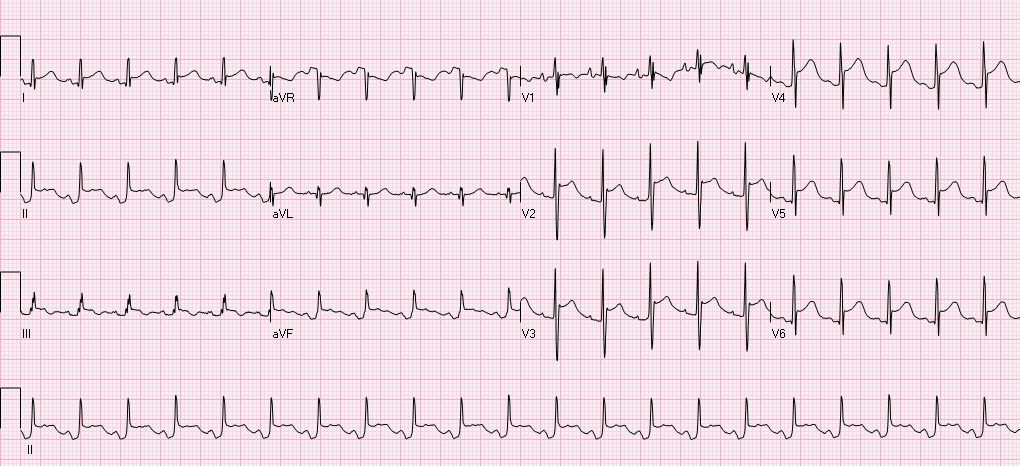
Clinical context: This is a 20s year-old male who presented to the ED after GSW to the thorax. He lost pulses in transport, and underwent ED thoracotomy, cardiac massage and aortic cross clamping with ROSC, and subsequent ex-lap. He has been in the ICU with complications including respiratory failure, renal failure, hemorrhagic shock, and multiple returns to the operating room for intrabdominal injuries. The following EKG was obtained over the weekend due to ST elevation noted on cardiac telemetry. Automated read notes sinus tachycardia, ****ACUTE MI/STEMI****
Let's systematically review this ECG. The ventricular rate is 126, there is a p wave before every QRS - sinus rhythm, QRS is upgoing in I, II - normal axis, PR, QRS intervals appropriate, QTC prolonged at 492, there is ST elevation in I, II, III, aVF, V2-V6 with concomitant PR depressions, reciprocal ST depressions and PR elevations in aVR and V1. This is a classic ECG for PERICARDITIS. The patient subsequently had cardiac ultrasound that demonstrated a small effusion as well. Remember that classic findings of pericarditis include widespread ST elevation and PR depression with reciprocal changes in aVR +/- V1. Life in the fast lane review of pericarditis While there are many causes of pericarditis, this patient has several underlying risk factors including chest trauma, surgery, and possible infection secondary to limited sterility in the emergency setting. While the reported incidence of acute pericarditis after general thoracic surgery is very low, I was not able to identify any recent literature addressing the incidence of pericarditis after ED thoracotomy in patients without penetrating cardiac injuries. In patients with penetrating cardiac injury delayed secondary cardiac injuries and complications occur at at rate of ~50%. Colchicine is noted to be used as pericarditis prophylaxis in major cardiac surgery and transplant, this could be considered in the ED setting, however the logistics and lack of evidence as to how common this complication is could limit benefit. Complications of ED Thoracotomy include:
Upon return to the OR the day after thoracotomy this patient was noted to have ongoing bleeding from internal mammary arteries, but no damage to coronary arteries or other cardiac damage. References: Imazio, M., Gaita, F., LeWinter, M. Evaluation and Treatment of Pericarditis A Systematic Review. JAMA. 2015;314(14):1498-1506. Fallahnejad M., Kutty AC., Wallace HW. Secondary lesion of penetrating cardiac injuries: a frequent complication. Ann Surg. 1980;191(2):228. Alraies MC, AL Jaroudi W, Shabrang C, et al. Clinical features associated with adverse events in patients with post-pericardiotomy syndrome following cardiac surgery. Am J Cardiol. 2014 Nov;114(9): 142630. Keller D, Kulp H, Maher Z, et al. Life after near death: Long term outcomes of Emergency department thoracotomy survivors. J Trauma Acue Care Surg. 2013 May;74(5):1315-20. HPI: A previously healthy, incarcerated, 43 year old Asian American male presented to the ED after a syncopal episode with subsequent VF arrest. The patient is successfully defibrillated. After ROSC the following EKG is obtained: Normal rate, regular rhythm, sinus P waves in from of QRS. normal PR, normal QRS width, axis, amplitude, progression. ST elevation in V1, V2, inverted T waves in V2, normal QTc.
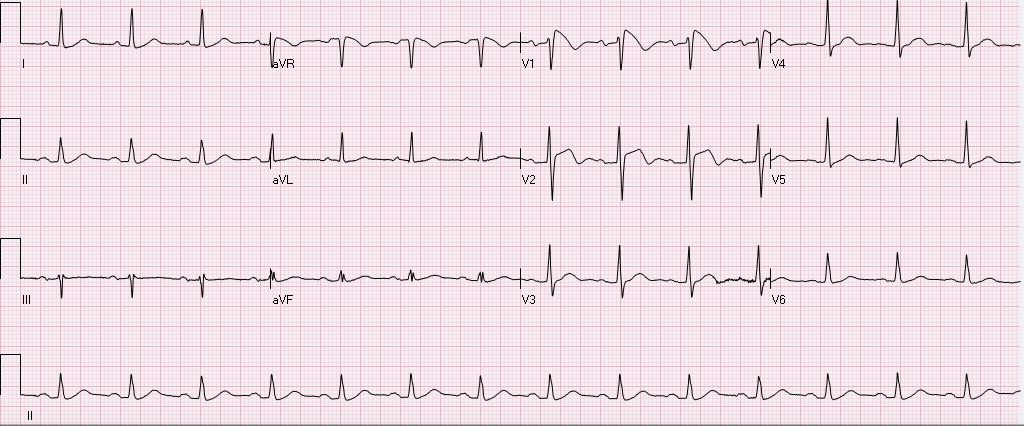
After obtaining this EKG the patient was rushed to the cath lab, no obstructive coronary lesions were identified. What is the diagnosis, and what is the treatment? Is this finding always pathological? The diagnosis is Brugada syndrome. - syndrome is a constellation of Brugada pattern EKG + CLINICAL SYMPTOMS Brugada Pattern EKG: -RBBB pattern in V1 (rSR', terminal positive QRS complex) -high take off, upward convex, ST elevation in V1 and V2 -inverted T waves in V1 and V2 Clinical Symptoms: syncope, +/- palpitations, unexplained VF/arrest, family history of sudden death. Brugada Syndrome: -due to poorly understood sodium chanellopathy. There is NO UNDERLYING STRUCTURAL HEART DISEASE. -except for V1-V2, the EKG is usually normal. -Brugada pattern on EKG can be transient, and can be unmasked by physical stressors, medications, metabolic derangements, and ischemia. Treatment: ICD is indicated for patients with Brugada syndrome. Brugada Pattern EKG is NOT ALWAYS pathalogical. -Brugada pattern EKG can be a normal variant, especially in a patient without risk factors, symptoms, and the pattern is an incidental finding during a non-cardiac workup. -Brugada pattern can also be seen in severe hyperkalemia, sodium-channel blocker toxicity, propofol infusion syndrome, right ventricular pathology or injury. Patients who are incidentally found to have Brugada pattern EKG without cardiac symptoms are at low risk for sudden cardiac death. These patients should be educated on finding, referred to cardiologist, and given careful follow up precautions if they develop syncope, palpitations, chest pain, or other cardiac symptoms. A careful family history to elucidate family members with sudden cardiac death is warranted. There is some risk if the patient has Brugada EKG pattern without symptoms, but does have a family member who experienced sudden cardiac death. These patients should be referred to a cardiologist, and may undergo provocative testing to induce VT/VF, although this is controversial. References: 1. Littmann, L. Monroe, MH., Kerns, WP., Svenson, RH., Gallagher, JJ. Brugada syndrome and "Brugada sign": clinical spectrum with a guide for the clinician. Am Heart J. 2003 May;145(5):768-78. 2. http://lifeinthefastlane.com/ecg-library/brugada-syndrome/ HPI: 83 year old caucasian male with a past medical history of atrial fibrillation, COPD, HTN, metastatic prostate cancer, presented to ED after a ground level fall, found to have altered mental status, cerebral edema with midline shift, no intracranial bleeding. EKG: Auto read: Demand pacemaker; interpretation is based on intrinsic rhythm. Atrial fibrillation with premature ventricular or aberrantly conducted complexes. Cannot rule out Inferior infarct, age undetermined. ST & T wave abnormality, consider anterolateral ischemia or digitalis effect. Abnormal ECG. No previous ECGs available.
Let's discuss this EKG. Ventricular rate is in the 60-70s, rhythm is definitely not sinus, as there are not a p wave before every QRS. The P waves, in fact, are absent. Axis is normal (upgoing QRS in I & aVF). The QRS is upgoing in Lead I suggestive of left ventricular pacing. QRS is not wide, QT is not prolonged. There are deep negative T waves in II, III, aVF, V4, and V5. There is normal R wave progression. Deep T waves in this EKG are a result of a phenomenon known as Cardiac Memory. These are NON-ISCHEMIC T wave inversions that are a result of repolarization abnormalities in the setting of intermittently wide QRS. So what causes these non-ischemic t-wave inversions? Well, first the QRS must become intermittently wide, as is seen in demand pacing (such as in the patient in this case), WPW, prolonged VT, or intermittent LBBB. Then, as the QRS becomes narrow again, the T waves become negative in the leads where QRS was wide. There is a lag in resolution of the repolarization abnormality, which is likely channel related (but poorly understood). The persistence of T wave inversion depends on how frequently the QRS is wide, or in this case, how frequently the heart is LV paced. Basically the T waves are slow to normalize after an episode of widened QRS. There is a broad differential diagnosis for T wave inversion, including subendocardial ischemia, acute CNS bleeds, acute adrenergic stress, PE, metabolic abnormalities, and drug effects. Because of the broad differential, new diffuse T wave inversion should always focus on the "worst first", and in general cardiac memory is a diagnosis of exclusion. Recognizing this characteristic post-pacing T-wave morphology can be a valuable piece of information in your clinical decision making. Ischemia workup is not indicated based on the EKG alone. This transient EKG finding, in conjunction with negative serum cardiac enzymes, absence of chest pain/cardiac complaints, makes cardiac memory the most likely cause of the EKG abnormality. Don't fear the deep inverted T waves in demand pacing! References: Littman, L., Fermant, A. Large T-Wave Inversion in a Patient With a Pacemaker. Arch Intern Med. 2011 Aug 8;171(15):1314-16. |
EKG ChallengeAuthorER residents on Dr. Littmann's cardiology service present an interesting EKG and core concepts from Dr. Littmann. Archives
January 2016
Categories
All
Disclaimer: All EKG's and images are the sole property of CMC Emergency Medicine Residency and cannot be reproduced without written consent. Patient identifiers have been redacted/changed or patient consent has been obtained. Information contained in this blog is the opinion of the authors and application of material contained in this blog is at the discretion of the practitioner to verify for accuracy.
|

 RSS Feed
RSS Feed
