|
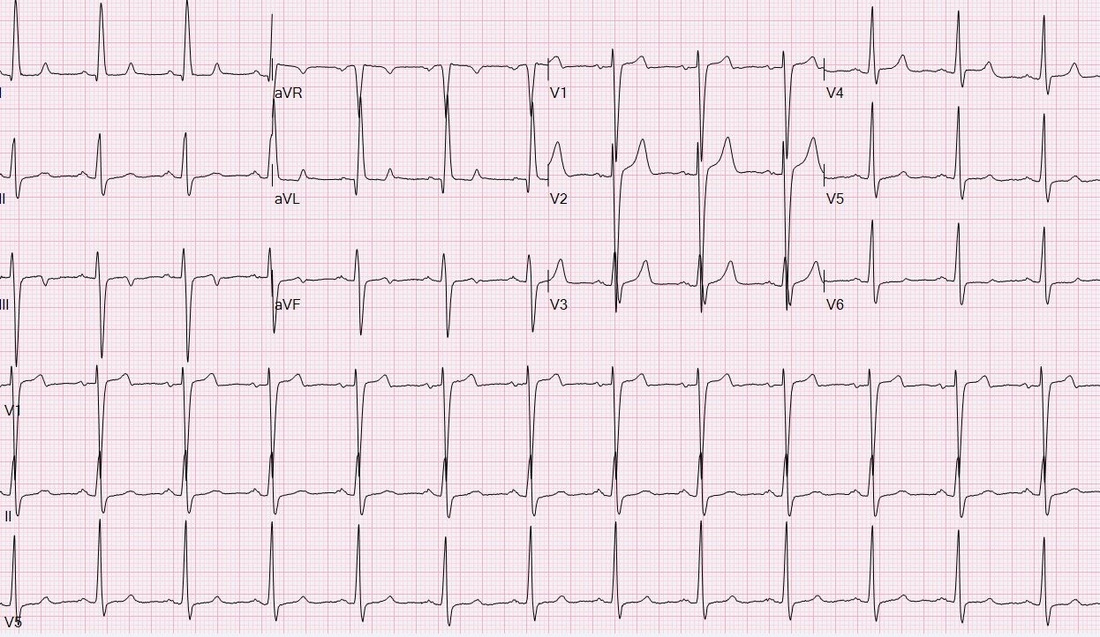
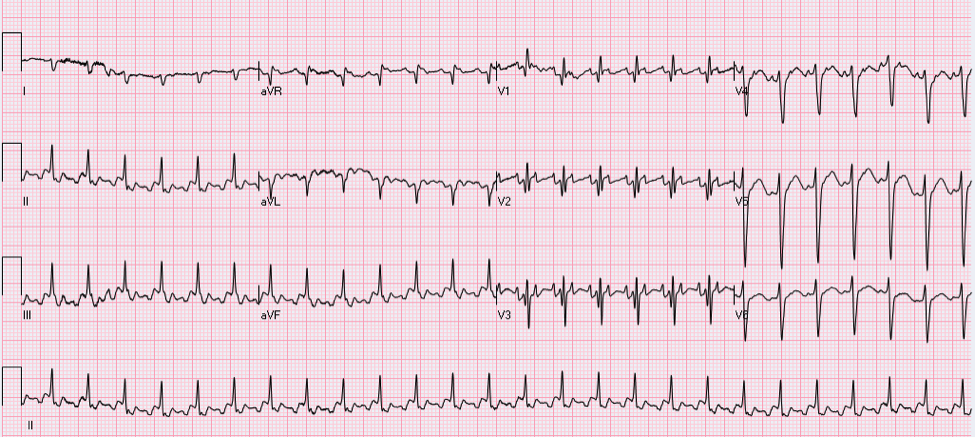
HPI: Patient is a 50 yo F with a history of ESRD s/p failed renal transplant now on hemodialysis who had onset of GI bleeding with associated lightheadedness and hypotension. An EKG was obtained. EKG: Question: What finding on this EKG warrants further management? EKG Interpretation: Normal sinus rhythm at a rate of 77, normal PR interval, normal QRS, normal axis, LVH (significantly increased voltages), narrow based, peaked T-waves, T-wave inversions in leads III and aVF. Discussion: The narrow based, peaked T-waves present in this patient’s EKG, most evident in leads V3-V4, indicate probable hyperkalemia in this patient who is at risk for elevated potassium given her ESRD. The T-wave abnormalities in this EKG are somewhat subtle, but the narrow, “pinched down” bases of the T-waves should warn you of hyperkalemia. This patient’s potassium level was found to be 6.9 and was appropriately treated. Pro-tip:
Potassium can be the great imitator on EKGs because it can cause a wide variety of abnormal EKG findings, including (but not limited to): • Peaked T-waves (often the earliest EKG sign of hyperkalemia) • Prolonged PR interval • Loss of P waves • AV block • Broad QRS complexes with abnormal morphology • Sine waves (usually with extremely severe hyperkalemia) Management:
For patients with ESRD on hemodialysis, dialysis is the definitive treatment for hyperkalemia. Typical management of hyperkalemia (for K>6.0 or EKG changes) includes**: • Calcium (either IV calcium gluconate or calcium chloride), which stabilizes cellular membranes by antagonizing the effect of potassium on membrane potential. Usually reserved for K>7.0 or EKG changes. • Insulin to promote the movement of potassium into cells. • Albuterol and Sodium bicarbonate can also be used to promote the movement of potassium into cells depending on potassium levels. • Kayexalate (Sodium polystyrene sulfonate) can be used to promote potassium elimination from the body, however this has no role in the acute management of hyperkalemia with EKG changes. **Caution in patients with DKA because total body potassium may actually be low and aggressive management of hyperkalemia can result in hypokalemia** By: Krystin Thomas, PGY1 Resources: • Stone, CK. Fluid, Electrolyte, and Acid-Base Emergencies. In Current diagnosis & treatment emergency medicine. 6th ed. New York: McGraw-Hill; 2008. • Burns, E. Hyperkalemia [Web log post] Retrieved August 28, 2015, from http://lifeinthefastlane.com/ecg-library/basics/hyperkalaemia/
0 Comments
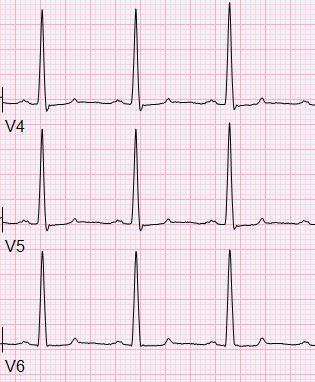
HPI: 90 y/o woman h/o sick sinus syndrome, AF, and a pacemaker presents with atypical CP. Troponins are negative, CTPA is negative for PE. She denies palpitations, shock-like sensations, or chest wall contractions. Palpated HR corresponds with QRS complexes on the monitor. EKG: Question:
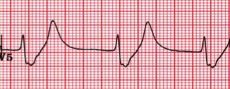
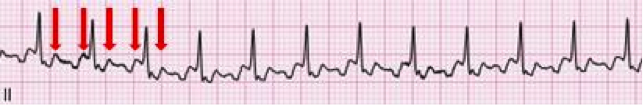
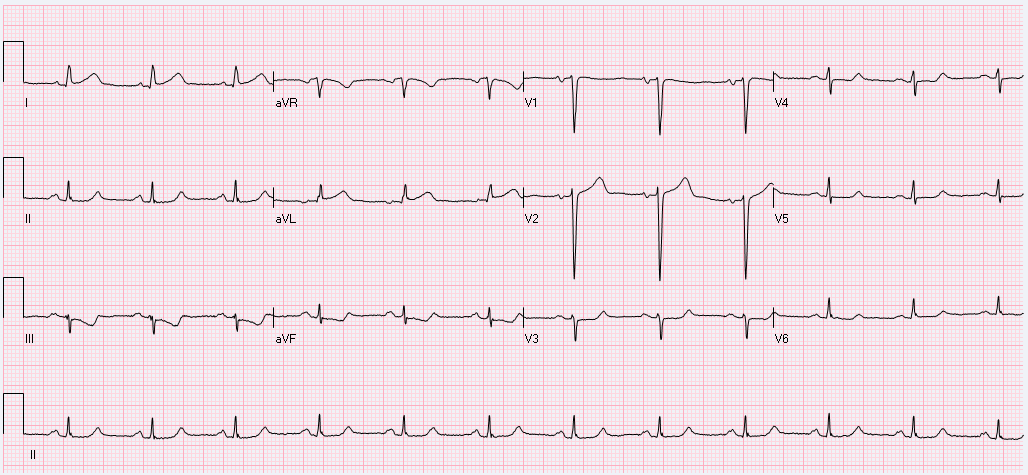
What's going on with this pacemaker? Is the malfunction the cause of her symptoms? EKG interpretation: Ventricular paced rhythm at a rate of approximately 70. QRS complexes are wide. QRS in V1-V6 are predominantly downgoing as are II, III, and aVF consistent with RV pacing. P waves with variable PR interval are seen in II, III, aVL, aVF, and some of the V leads. Pacer spikes are inconsistently seen in I, II, V1-V3. Discussion: This patient presents with atypical chest pain and an apparent pacemaker malfunction. Her pulse corresponds to her QRS complexes, so what's actually going on? As it turns out, this patient is being paced appropriately at her predetermined rate. Interrogation of her PM revealed normal functionality including normal lead impedance (high impedance can signify a fractured PM wire, low impedance can signify cracked insulation). The issue with the EKG here is that some 12 lead machines pick up small pacer spikes in the surface EKG and amplify them so they are visible to the provider. Unfortunately, some machines will only intermittently detect and amplify these spikes due to their signal processing and occasionally will pick up on interference and amplify it as a pacer spike. If you look closely at aVL, she has tiny pacer spikes before her QRS that the machine did not amplify. In this case, the machine used to record the EKG was a GE Marquette MAC 5000. Note that the QRS complexes in the V1 rhythm strip are all identical despite the intermittent pacer spikes suggesting that the pacemaker is actually generating the impulse for each QRS. Management: - Treat the patient as you normally would... labs, CTPA, ASA, NTG, etc as appropriate - If PM malfunction is suspected, interrogate the device. - Consider machine artifact in a patient with "intermittent" pacing who has consistent QRS complexes on their EKG and an regular HR - CXR can be very useful for identifying pacemaker type and manufacturer; focus on the identification tag on the device By: Dr. Andrew Godfrey, PGY1 References: 1. Butscek R, Farrell RM, Littmann. ECG quiz: what is the cause of the apparent pacemaker malfunction? J Electrocardiol. 2013 Mar-Apr;46(2):108-9. 2. Littmann L, Farrell RM. Potential misinterpretations related to artificial pacemaker signals generated by electrocardiographs. J Electrocardiol. 2015 Jul-Aug;48(4):717-20 HPI: 50 y/o male with hx of COPD, heroin use, and recently diagnosed cor pulmonale presents with 3 weeks of lower extremity edema. No chest pain, shortness of breath, or palpitations. An EKG is obtained in the emergency department. Question: What does this EKG tell you about the etiology of this patient’s lower extremity edema? EKG Interpretation: 2:1 atrial flutter with a rapid ventricular response at a rate of 156, narrow QRS (may appear wide due to buried P-waves), right axis deviation, RBBB. Discussion: The patient presents in 2:1 atrial flutter with a ventricular rate of 156, meaning that the atria are firing at a rate 2 times faster (approximately 312). The extra P-waves give the EKG baseline the typical “sawtooth” appearance of atrial flutter. Typical characteristics of atrial flutter:
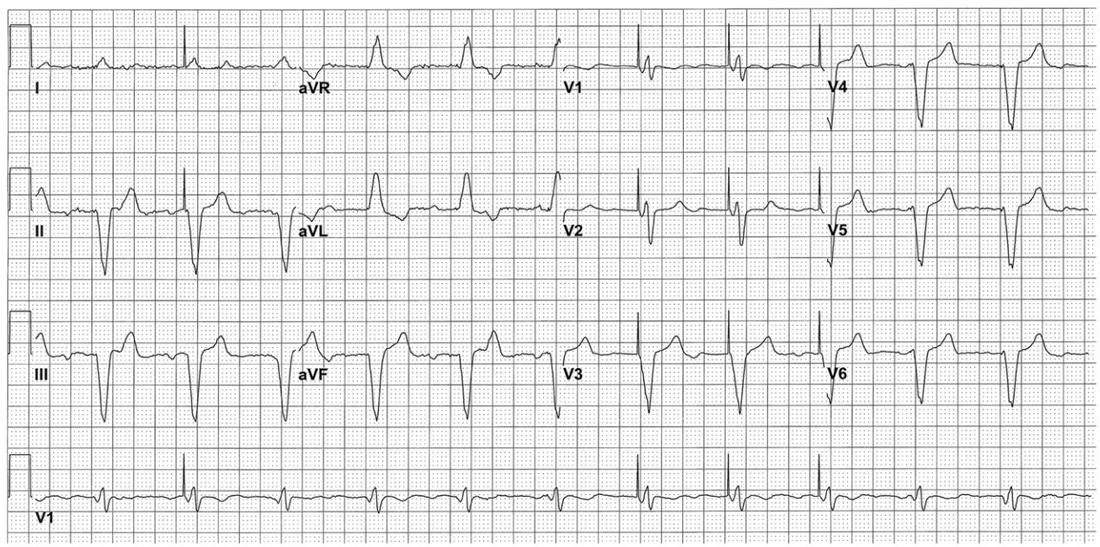
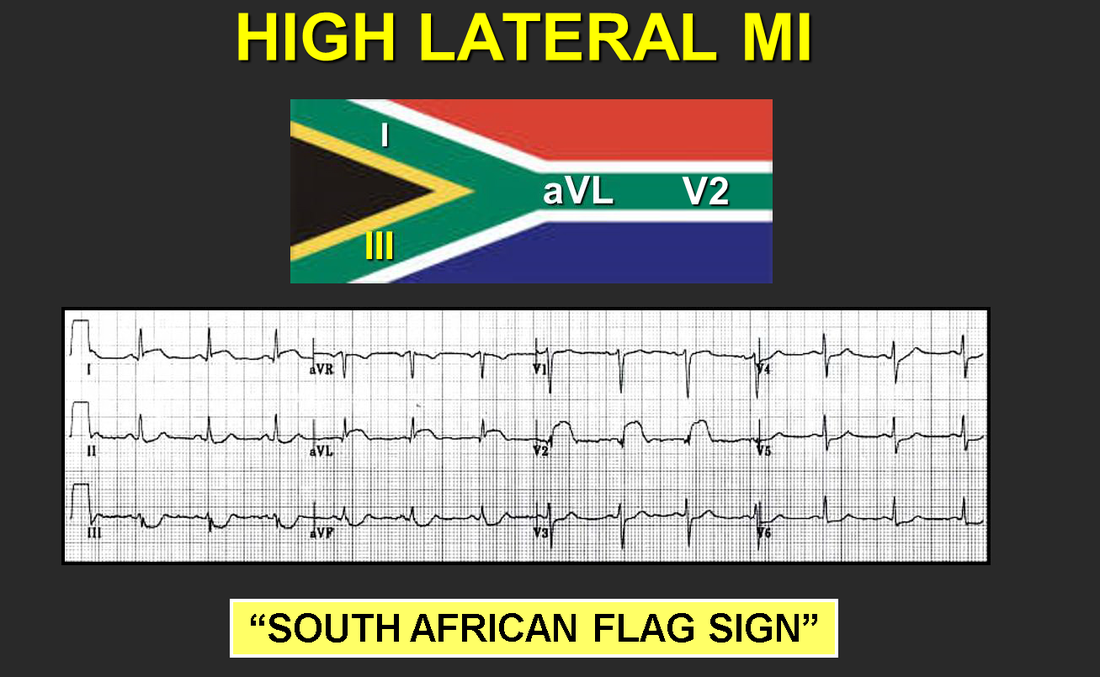
· Regular atrial rate – between 250-350 bpm · Sawtooth flutter waves – directed superiorly and most visible in leads II, III, and aVF · Atrioventricular block – usually at 2:1, but occasionally greater, associated with ventricular rate between 125-175 bpm Pro-tip: If you ever have difficulty distinguishing the buried P-waves of atrial flutter, you can block down the AV node with vagal maneuvers or Adenosine and the slowing of the ventricular rate will unmask the underlying atrial rhythm. Narrow-complex tachycardia at a rate of 130-170: suspect flutter!! Atrial flutter was the cause of this patient’s severe lower extremity edema extending to the scrotum and pre-sacral level. It is not uncommon for patients in atrial flutter to present with edema due the lack of forward flow through the heart secondary to atrial flutter. This patient’s atrial flutter is most likely a result of his severe cor pulmonale, his right atria and ventricle were found to be massively dilated on echocardiogram, predisposing patient to atrial flutter. In general, patients with right heart disease are more likely to get atrial flutter rather than atrial fibrillation, however “where there’s fib, there’s flutter” and these patients can exhibit episodes of a.fib as well. Management: If the patient is stable, the first priority is to achieve ventricular rate control with beta-blockers or nondihydropyridine calcium channel blockers. This patient was given a Diltiazem bolus and then placed on a drip which improved his rate into the 80s, although he was still in 2:1 atrial flutter. Long-term management options for stable patients can be divided into rate control or rhythm control. Rhythm control options: · Cardioversion is an option if patient is known to have been in this rhythm for < 48 hours, if > 48 hours patient requires either: a TEE without evidence of mural thrombus + Heparin or >= 3 weeks of anticoagulation prior to cardioversion (all patients need 4 weeks of anticoagulation post-cardioversion as well) · Catheter ablation for select patient’s (larger right atrium size correlates with lower success rates) Rate control options: · Calcium channel blockers · Beta-blockers By: Dr. Krystin Thomas, MD References: 1. Tintinalli JE. Cardiac Rhythm Disturbances. In: Tintinalli's Emergency Medicine a Comprehensive Study Guide. 7th ed. New York: McGraw-Hill; 2011. 2. Burns, E. Atrial Flutter [Web log post] Retrieved August 15, 2015, from http://lifeinthefastlane.com/ecg-library/atrial-flutter/ HPI: 57 y/o woman with remote hx of CABG/PCI presents with 2 hrs of 6-10/10 substernal chest tightness and SOB. No recent cardiac events/complaints. Initial troponin is 1.48. EKG Interpretation: normal sinus rhythm at a rate of 71 with a normal axis. Narrow QRS complexes throughout, normal intervals. Mild ST elevation in I, aVL, and V2. Inverted T wave in III with mild ST depression as well. No previous EKG available for comparison. Discussion: Although this patient does not have an obvious STEMI on their EKG, there is mild elevation in I, aVL and V2 with reciprocal changes in III, a pattern similar to the South African flag. Concern should be high for a high lateral MI which is an area of that is poorly represented by standard EKG lead placement. In this case, the patient had an acute thrombotic occlusion of a diagonal branch of the LAD artery. On the initial EKG, the patient has lower voltages in their limb leads as well as V3-V6. Although they don’t have frank ST elevation ≥ 1 mm in any lead other than V2, their mild ST elevation should be concerning given the low(er) QRS voltage. Move one of the V leads higher into the left axilla (2-3 interspaces) to obtain a tracing of the high lateral wall. Make sure to discuss with Cardiology your concern for a potential STEMI despite the lack of qualifying ST elevation.
Management: - Obtain EKG tracing of high lateral wall - Labs including troponins as well as CXR - MONA, heparin - Cardiology consult emphasizing the concern for ST changes in the setting of low QRS voltage - Consider emergent cath for patients with persistent chest pain and persistent ST changes By: Dr. Andrew Godfrey |
EKG ChallengeAuthorER residents on Dr. Littmann's cardiology service present an interesting EKG and core concepts from Dr. Littmann. Archives
January 2016
Categories
All
Disclaimer: All EKG's and images are the sole property of CMC Emergency Medicine Residency and cannot be reproduced without written consent. Patient identifiers have been redacted/changed or patient consent has been obtained. Information contained in this blog is the opinion of the authors and application of material contained in this blog is at the discretion of the practitioner to verify for accuracy.
|

 RSS Feed
RSS Feed
