|
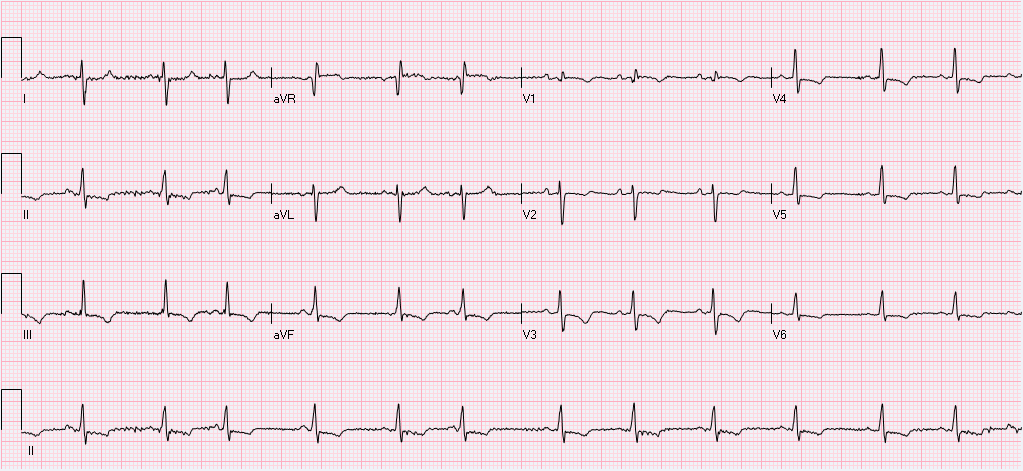
HPI: The patient is a 66 yo F with PMH CHF (TTE 9/2009 with LVEF 50%, RVSP 42), CAD s/p cath ( no stents), DMII, HLD, HTN, and morbid obesity who presents with a cc of abdominal swelling. Onset was 3 months prior to presentation with persistent worsening since that time. She denies any SOB or chest pain/diaphoresis and denies any home O2 use. She does endorse significant weight gain and lower extremity swelling during the same time period. Otherwise, ROS is significant for a fall yesterday, reported to be mechanical without LOC. Labs: remarkable for BNP >2000, no prior value. Troponin 0.01. EKG: Interpretation: Normal sinus rhythm. Rate 76. Right axis deviation with deep S wave in lead I. Normal PR, QRS, and QT intervals. T wave inversions noted in II, III, avF, and all precordial leads. R wave progression which is remarkable for predominantly upgoing QRS in lead V1 with qR complex. As compared to prior EKG(2009), Afib is not present on current. All of the above findings are new.
Conclusion: The patient was subsequently admitted for new onset CHF. Following the echocardiogram which demonstrated the above, the patient was gradually diuresed with plans for RHC to further clarify RVSP with the goal of starting pulmonary vasodilator therapy. RHC was performed 9 days after admission following volume optimization and demonstrated PA 78/36. Pulmonary vasodilator therapy was initiated and the patient was discharged home on these medications. Teaching Points: This patient’s EKG from admission is very consistent with right ventricular hypertrophy and severe pulmonary hypertension. This is evidenced by the new right axis deviation. Further evidence is the qR complex with predominantly upgoing QRS in V1 and T wave inversions inferiorly and in the anterior chest leads. EKG evidence of Pulmonary Hypertension:
Blyth et. al. Quantitative estimation of right ventricular hypertrophy using ECG criteria in patients with pulmonary hypertension: A comparison with cardiac MRI. Pulm Circ. 2011. 470-4. Whitman et al. Validity of the surface electrocardiogram criteria for right ventricular hypertrophy: the MESA-RV study. J Am Coll Cardiol. 2014 Feb 25; 63:672-81. Blog by Dr. Jaron Raper
0 Comments
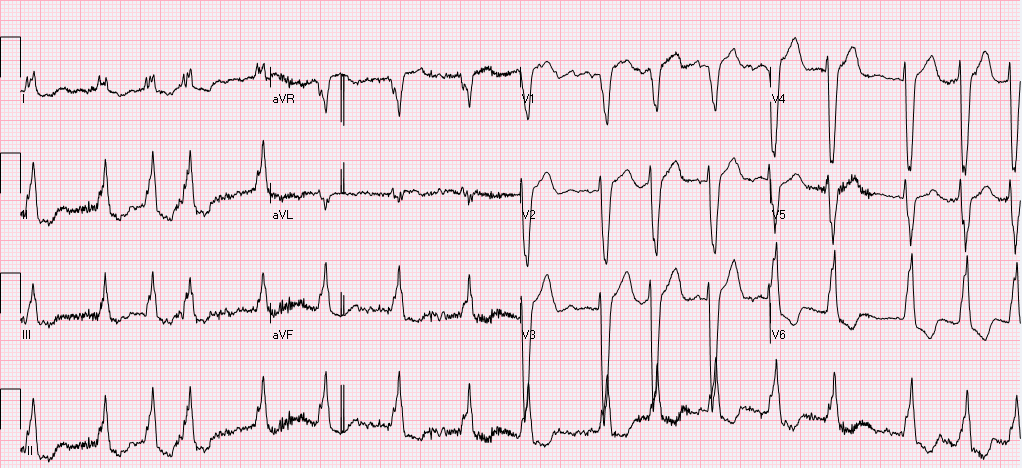
HPI: The patient is a 71 year old male with PMH of ischemic cardiomyopathy (HFrEF 25%) and AICD in place, moderate mitral regurgitation, permanent atrial fibrillation (rate control and fully anticoagulated), HTN, and COPD who presents to the ED with worsening shortness of breath following a fight with his girlfriend a few hours before. He denies any chest discomfort or palpitations but does endorse presyncope with tunnel vision. At onset, he turned his home O2 up to 3L from 1L. Upon EMS arrival, he received solumedrol and a Duoneb treatment without improvement. Upon arrival to the ED the patient was tripoding and in severe respiratory distress. A trial of BiPap in the emergency department was unsuccessful 2/2 continued distress and increased work of breathing, and the patient was subsequently intubated. Exam: significant for tachypnea to 29. Otherwise VS wnl.. Tripoding and accessory muscle use. Irregularly irregular rhythm with blowing holosystolic murmur 3/6 loudest at the left sternal border. CXR: - Interpreted as severe pulmonary edema EKG: EKG (prior to intubation): Atrial fibrillation. Rate 90’s. Normal axis. QRS >140ms. QS in V1 consistent with LBBB. High frequency oscillatory pattern/respiratory artifact noted as highlighted above, consistent with severe respiratory distress. No Sgarbossa criteria are present. Occasional pacer spike noted.
Relevant Laboratory Data: BNP 1400 from prior 1000, Troponin 0.00à0.06, spot cocaine negative Echo: Left atrium and ventricle are dilated. LVEF 25-30% with septal akinesis. Normal valvular function, however prior echo does report 3+ mitral regurgitation. Otherwise unchanged from prior. Interval History: The patient was admitted to MICU, where he was subsequently weaned from the ventilator and extubated within hours of admission following afterload reduction and IV diuresis. Chart review did demonstrate this to be the third admission in the last 2 months for similar symptoms requiring intubation. Prior AICD interrogations demonstrated afib with RVR with a rate of >200, presumed to be the inciting event for respiratory failure. Current management plan (pending) is for repeat AICD interrogation, and nuclear perfusion stress testing to rule out new ischemia. Subsequently the patient will be converted to a BiV pacer with plans for ablation of the His-bundle which should prevent further episodes of RVR and will result in complete pacer dependence. Teaching Points: Respiratory Artifact
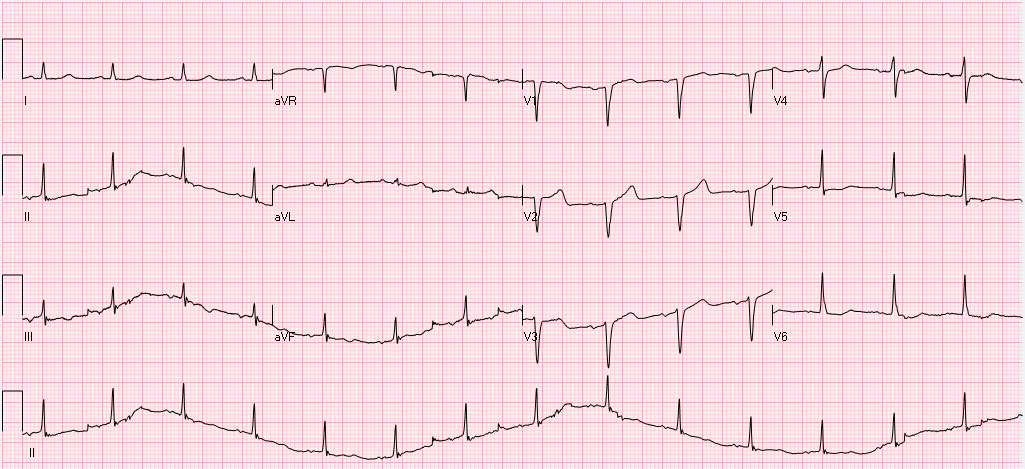
Littman L, Rennyson SL, Wall BP, Parker JM. Significance of Respiratory Artifact in the Electrocardiogram. Am J Cardiol. 2008 Oct 15;102(8):1090-6. doi: 10.1016/j.amjcard.2008.05.061. Epub 2008 Jul 25. Blog by Dr. Jaron Raper HPI: The patient is a 69 yo Male with suttering chest pain for the last 8 or 9 days who woke up initially with severe stabbing 10/10 substernal chest pain with concurrent shortness of breath. He did not seek immediate medical attention, but continued to have recurrent episodes of chest pain over the course of the next week which were both exertional and nonexertional. Throughout this same time period he reports fatigue and SOB for which he sought evaluation at his PCP, who referred him to the emergency department. Exam: significant for a systolic ejection murmur 3/6 in intensity heard best over the left sternal border and radiating to the axilla. Radiation is also noted to the carotids bilaterally. The second heart sound is only mildly decreased. Hemoccult positive. Labs: Notable for normocytic anemia with Hgb 7.5. Initial troponin was 0.80 and peaked at 1.14. EKG: Interpretation: Normal Sinus rhythm. Rate 89. Normal axis. Normal PR, QRS, and QT intervals. T wave inversions noted in II, III, and aVF. Poor R wave progression and cannot rule out remote anteroseptal MI evidenced by Q waves in V1,V2, V3.
Cath: The patient was subsequently cath’d and found to have 100% mid-distal RCA occlusion which is consistent with inferior ischemia previously noted on EKG. LAD ostial 50% and mid 50% stenosis. Echo: significant for mild aortic stenosis with mean gradient 22 mmHg. Conclusion: Following catheterization, no stenting was performed and plans for follow-up with GI for colonoscopy to determine source of occult bleed. Cath did confirm a remote RCA infarct presumed to be exacerbated by the patient’s anemia. Aortic stenosis was not considered severe enough to generate Heyde’s syndrome (mean gradient of <40mmHg) Teaching Points: Heyde's Syndrome
Vincentelli A, Susen S, Le Tourneau T, Six I, Fabre O, Juthier F, Bauters A, Decoene C, Goudemand J, Prat A, Jude B. Acquired von Willebrand syndrome in aortic stenosis. N Engl J Med. 2003;349(4):343. Blog by Dr. Jaron Raper |
EKG ChallengeAuthorER residents on Dr. Littmann's cardiology service present an interesting EKG and core concepts from Dr. Littmann. Archives
January 2016
Categories
All
Disclaimer: All EKG's and images are the sole property of CMC Emergency Medicine Residency and cannot be reproduced without written consent. Patient identifiers have been redacted/changed or patient consent has been obtained. Information contained in this blog is the opinion of the authors and application of material contained in this blog is at the discretion of the practitioner to verify for accuracy.
|


 RSS Feed
RSS Feed
